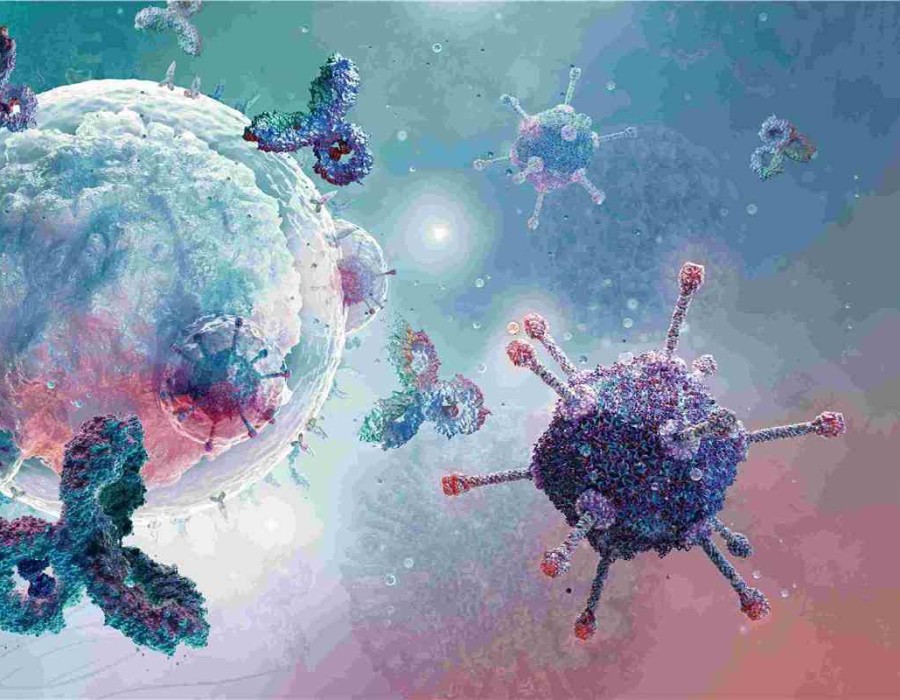
In the past ten years, the number of antibody drug conjugate (ADC) entering clinical trials has steadily increased. Currently, 9 ADCs have been approved, of which 5 are used for hematoma and 4 for solid tumor treatment. After more than 20 years of development, ADC biopharmaceuticals are becoming the main force in the treatment of cancer.
Currently, one of the most important challenges when designing a good ADC drug is to maximize its effectiveness while minimizing the non-target toxicity. In order to achieve a balance between safety and effectiveness, it is necessary to adjust and optimize each of the three structural elements of ADCs: antibody backbone, payload (cytotoxin), and a combination (linker) between them.
Antibody Backbone: The Starting Point for ADC Design
l Selection of antigen specificity
Since the mechanism of ADCs begins with the binding of target cells, the antibody should have high specificity for the target antigen. Ideally, the antigen should be overexpressed on the surface of tumor cells and not expressed (or very low) in normal tissues. Lack of high specificity or cross-reaction with other antigens will cause unpredictable side effects and reduce the treatment window.
Upon binding with the antigens on the surface of the target cells, ADCs are internalized and transported to the lysosome, where ADCs are subsequently degraded to release the payload. The degree of internalization depends on the affinity of the antibody to the target and antigen density. The optimal affinity depends on the nature of the target. High internalization is not necessarily beneficial to the treatment of solid tumors, because the rapid degradation of ADCs limits their ability to penetrate tumor masses. Uninternalized ADCs can also play a therapeutic role through the so-called "bystander effect", that is, the payload can penetrate the cell membrane of adjacent cells, which is very important for the treatment of solid tumors.
l Using bispecific antibodies
The specificity of binding to target cells can be improved by using a bispecific antibody. For example, bispecific ADCs targeting HER2 and prolactin receptor (PRL-R) have been shown to kill target cells (expressing both HER2 and PRL-R) more effectively than ADCs only targeting HER2, indicating rapid internalization and lysosomal degradation. In this case, using the bispecific antibody helped reduce unexpected toxicity in patients with low levels of HER2 expression.
l Selection of antibody size/fragment
Most anti-tumor ADCs are based on IgG1 antibodies, partly because these molecules can trigger Fc-mediated immune functions such as ADCC, CDC, and ADCP. However, most ADCs targeting solid tumors have not progressed beyond phase 2 clinical trials. The limited penetration rate in solid tumors is one important reason, affected by the size of IgG. In addition, excessive binding of FcRn can cause ADCs to return to the extracellular circulation, increasing exposure in healthy tissues, which not only limits the release of intracellular payloads but may also cause off-target toxicity. FcγR cross-reacts with endothelial cells and the immune system, and may also cause off-target toxicity. To make up for these shortcomings, recent studies have explored the efficacy of using smaller binding formats, such as antigen-binding fragments (Fab), single-domain antibody fragments (VHH), and single-chain antibodies (scFv).
Linker: The Key Factor in ADCs
The linker plays a key role in ensuring that the payload remains attached to the antibody during the systemic circulation and is then released after ADC internalization. Most ADCs are characterized by a cleavable linker, which releases cytotoxins through reduction, acidity, or proteolysis of the linker according to the physiological environment of the cell. On the other hand, for ADCs with non-cleavable linkers, the antibody would need to be degradedly completely after ADC internalization for the payload to be released.
l Lysine conjugation
The first-generation ADC drugs are based on lysine conjugate. A large amount of lysine in the structure of the antibody causes the wide heterogeneity of ADC. Mylotarg, the first ADC approved by the FDA for the treatment of acute myeloid leukemia, uses calicheamicin conjugated with the anti-CD33 monoclonal antibody through the side chain of lysine. However, about half of the drug is composed of unbound antibodies. These "naked" monoclonal antibodies compete with the conjugated form of ADC for target binding, limiting the effectiveness of the drug.
Mylotarg voluntarily withdrew from the market in 2010. Subsequentt clinical trials found that compared with chemotherapy alone, Mylotarg has no addition benefit and increases fatal toxicity, mainly due to the non-specific release of its acid-cleavable linker and payload. Mylotarg was re-approved in 2017 after the dosage regimen was changed.
l Cysteine conjugation
Most approved ADCs, including Adcetris in 2011 and all ADCs approved in 2019/2020, are based on cysteine binding. It is less heterogeneous compared with lysine binding. And because of a more predictable attachment site, the risk of blocking the antigen-binding region is also lower.
l Site-specific conjugation
Further improvements have been achieved through the use of site-specific conjugation technology. Although all ADCs currently approved use traditional lysine or cysteine-based conjugation, the use of site-specific binding strategies for ADCs in clinical development has increased significantly in recent years. There are many ways to achieve this, including the use of engineered cysteine, unnatural amino acids, enzyme-assisted ligation, and sugar chain remodeling. With these ADCs, the homogeneity of the product is greatly increased, making the treatment safer, more effective, and more targeted.
Cytotoxic Payload: ADC Tumor-Killing Nuclear Warhead
Most of the payloads are small hydrophobic molecules. Once released, they can pass through the biomembrane and disrupt key cellular processes to cause cell death. The most commonly used molecules are tubulin inhibitors, such as Auristatins (MMAE,MMAF, PE) and Maytansine, which account for more than half of ADCs in clinical development and, on the market. Other cytotoxic payloads with different action mechanisms include DNA alkylating agents and cross-linking agents, topoisomerase I inhibitors, and RNA polymerase inhibitors.
l Selection of drug-to-antibody ratio (DAR)
The optimal drug-to-antibody ratio (DAR) of ADCs depends on the effectiveness of the payload. For ADCs containing Maytansine, a standard DAR is about 4: lower DAR may cause loss of activity, while higher DAR often leads to toxicity.
Although ADC has a higher therapeutic index compared with traditional chemotherapy, there is still a need to broaden the window between efficacy and toxicity. Scientists are testing different methods to achieve this goal. One strategy is to use extremely powerful toxins, such as Pyrrolobenzodiazepine (PBD), with a DAR of around 2 to reduce the minimum effective dose required. In contrast, other ADC drugs, such as the already marketed Adcetris (DS-8201a) and Trodelvy (Sacituzumab govitecan), use lower effective payloads with a DAR of about 8 to reduce toxicity. With the development of technology, there is no fixed value for DAR, and the optimal DAR will depend on many parameters, mainly the hydrophilicity of the linker and the toxicity of the payload.
l Bystander effect of cytotoxin
Besides linkers, cytotoxic payloads also play an important role in the bystander effect. For example, MMAE is neutral and can pass through biological membranes, while MMAF produces metabolites with charged carboxy-terminal phenylalanine residues that cannot pass through biological membranes. Therefore, MMAF is less toxic to neighboring cells than MMAE.
l More types of payload
In addition to traditional cytotoxins, more and more payloads with new mechanisms of action are being incorporated into ADC design. These drugs include Toll-like receptors (TLR) and stimulators of interferon genes (STING) agonists, which are used to activate anti-tumor immune responses.
Summary
To design a good ADC drug, choosing the right combinations of antibody backbone, linker chemistry (conjugation technology), and payloads is crucial. Each of these components must be adjusted and optimized to obtain the correct balance between effectiveness and safety. For example, the ideal affinity of an antibody depends on the density of the antigen on the target; bystander activity may or may not be required; the optimal DAR depends on the effectiveness of the payload.
In the past ten years, ADCs have developed into a major biopharmaceutical category through improvements in all design aspects. There is still a lot of technical space and a strong market driving force for ADC drug design and further optimization. Nevertheless, many believe that the number and quality of ADCs will increase substantially in the next ten years.
References:
1. Martin De Cecco, Daniel N. Galbraith &Lisa L. McDermott. What makes a good antibody–drug conjugate? Expert Opinion on Biological Therapy. 2021 Feb.
2. Steven Coats, Marna Williams. etc. Antibody-Drug Conjugates: Future Directions in Clinical and Translational Strategies to Improve the Therapeutic Index. Clinical Cancer Research. 2019 Sep 15; 25(18): 5441-5448.
3. Nicolas Joubert, Alain Beck, Charles Dumontet, Caroline Denevault-Sabourin. Antibody-Drug Conjugates: The Last Decade. Pharmaceuticals (Basel). 2020 Sep 14; 13(9):245.
4. Cindy H Chau, Patricia S Steeg, William D Figg. Antibody-drug conjugates for cancer. Lancet. 2019 Aug 31; 394(10200):793-804.
5. Paul J Carter, Greg A Lazar. Next generation antibody drugs: pursuit of the 'high-hanging fruit'. Nat Rev Drug Discov. 2018 Mar; 17(3):197-223.



Comments