Autologous fat transfer (AFT) has become an increasingly popular technique in reconstructive and aesthetic surgery, offering a promising alternative to synthetic implants for volume restoration. Despite its wide use, the long-term reliability of fat transfer remains a subject of debate. This article reviews the current scientific understanding of the reliability of AFT, with a focus on its application in aesthetic procedures, clinical outcomes, and factors that influence fat graft survival. We also discuss advancements in technique, challenges in clinical practice, and potential strategies for improving graft retention and long-term results.
Autologous fat transfer, also known as lipofilling or fat grafting, involves the harvesting of adipose tissue from one area of the patient's body (typically via liposuction), followed by its purification and re-injection into areas requiring volume enhancement. AFT has gained substantial popularity in both reconstructive and cosmetic surgery due to its minimal invasiveness, natural results, and use of the patient’s own tissue, which eliminates concerns regarding immunologic rejection or material-related complications. Common applications of AFT include facial volume restoration, breast reconstruction, and buttock augmentation.
While the technique is widely utilized, questions remain regarding its long-term reliability, especially concerning the stability of grafted fat and its potential for resorption. This article aims to review the scientific literature on the reliability of autologous fat transfer, analyzing the factors that influence graft survival and offering insights into how these challenges can be addressed.
Mechanisms of Fat Graft Survival
Fat graft survival is contingent upon several biological processes that govern the engraftment of transplanted adipocytes. Upon injection, adipocytes are deprived of their original vascular supply, and the success of the graft depends on its ability to establish a new blood supply, a process known as neovascularization. For a graft to survive, the transplanted adipose tissue must transition from a hypoxic state to one with sufficient oxygenation and nutrient supply. Failure to achieve this may result in partial or complete resorption of the fat, leading to suboptimal or inconsistent results.
A key factor influencing the success of fat transfer is the method of graft harvesting, processing, and injection. Different techniques—ranging from mechanical to more sophisticated methods like enzymatic or centrifugation—affect the viability of the harvested fat cells and can, in turn, influence graft retention. Additionally, the location and depth at which the fat is injected play a role in its survival, with deeper injections often resulting in better outcomes due to improved vascularization.
Factors Affecting Fat Transfer Reliability
Several patient- and technique-related factors contribute to the reliability of autologous fat transfer:
- Graft Handling and Processing: The manner in which the harvested fat is processed and prepared before injection is one of the most critical determinants of graft survival. Overhandling or excessive centrifugation may damage adipocytes, leading to a higher rate of fat cell death. Conversely, gentler processing methods, such as manual aspiration and minimal centrifugation, tend to preserve fat cell viability, enhancing graft retention.
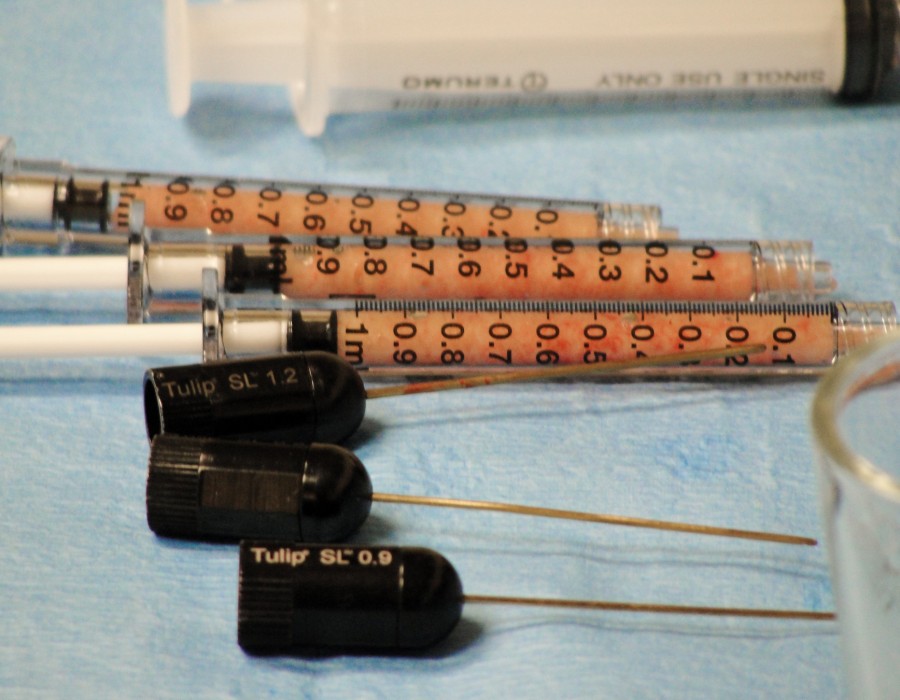
- Injection Technique: The technique used to inject the fat also plays a significant role in the survival of the graft. The distribution of fat in small, dispersed aliquots rather than large bolus injections has been shown to promote neovascularization and reduce fat necrosis. Additionally, a multi-layered injection strategy, where fat is placed at various depths in the recipient site, has been linked to better outcomes in terms of volume retention.
- Recipient Site Characteristics: The anatomical characteristics of the recipient site, including the tissue composition (muscle, skin, or bone) and the blood supply, can influence fat graft survival. Areas with poor vascularization may be more prone to fat resorption. Additionally, sites with minimal movement or low mechanical stress, such as the face, tend to exhibit better graft retention than high-mobility areas like the buttocks or breasts.
- Patient-Related Factors: Factors such as age, body mass index (BMI), and overall health can impact graft survival. Younger patients tend to experience better fat retention, likely due to more robust regenerative processes. Additionally, patients with higher BMI may have better outcomes, as their adipose tissue is often more viable and capable of supporting graft survival. However, excessive weight fluctuations can negatively impact long-term results.
- Postoperative Care: Postoperative care, including managing pressure on the grafted area and avoiding strenuous activity, is vital for preventing fat resorption. Compression garments, commonly used after breast augmentation or buttock procedures, may help maintain the shape and volume of the transferred fat by reducing tissue compression during the healing phase.
Challenges in Fat Graft Retention
Despite its advantages, fat transfer is associated with several challenges related to graft retention and long-term volume stability:
- Fat Resorption: Fat grafts typically undergo some degree of resorption postoperatively, with studies suggesting that around 30-50% of the transplanted fat may be reabsorbed within the first six months. Factors influencing resorption include graft size, injection technique, and the quality of the fat cells themselves. This resorption can lead to the need for secondary fat grafting procedures, which can increase the overall cost and complexity of treatment.
- Fat Necrosis and Cyst Formation: Another challenge is the potential for fat necrosis, which can occur when fat cells die due to inadequate blood supply or trauma. This can lead to the formation of lumps or cysts at the injection site, which may require additional surgical intervention. Techniques such as smaller injection volumes and improved fat processing have been shown to reduce the risk of fat necrosis.
- Long-Term Stability: Over time, the structural integrity of fat grafts may change, as the transplanted fat undergoes remodeling. This remodeling process may result in changes in volume, texture, or firmness, affecting the long-term aesthetic outcome. While many studies have reported stable results in the first year after fat transfer, the reliability of fat grafts beyond this period is less certain.
Advances in Autologous Fat Transfer
Recent advancements in fat transfer techniques have focused on improving graft survival and long-term outcomes:
- Stem Cell Enrichment: Recent studies have explored the addition of adipose-derived stem cells (ADSCs) to fat grafts to improve survival and regenerative potential. ADSCs have been shown to enhance neovascularization and tissue regeneration, potentially reducing fat resorption and improving graft stability. However, the clinical application of stem cell-enriched fat grafts is still in the experimental stages, with ongoing research needed to establish the safety and efficacy of this approach.
- Nanotechnology and Growth Factors: The use of growth factors, such as platelet-rich plasma (PRP), in combination with fat grafts has been investigated to promote fat cell survival and accelerate neovascularization. Furthermore, emerging technologies such as nanofat and microfat grafting aim to enhance the engraftment process by using smaller fat particles that are more easily incorporated into surrounding tissue.
- Improved Harvesting Techniques: Advances in liposuction technology, including the use of power-assisted or laser-assisted devices, allow for more efficient fat harvesting while minimizing trauma to adipocytes. Additionally, the development of tissue-specific harvesters, which selectively obtain the healthiest fat cells, has shown promise in improving the quality of the grafted tissue.
Autologous fat transfer represents a reliable and versatile option for volume restoration in both aesthetic and reconstructive surgery. However, its long-term success is influenced by various factors, including graft handling, injection technique, patient characteristics, and postoperative care. Although fat resorption and necrosis remain challenges, advances in technique, stem cell enrichment, and the use of growth factors offer promising solutions to enhance graft survival. Ongoing research and technological improvements will continue to refine fat grafting techniques, ultimately improving the reliability and predictability of this procedure in clinic practice.




Comments