How Does The COVID-19 Coronavirus Kill? What Happens When You Get Infected
 Bruce Y. LeeSenior Contributor
Bruce Y. LeeSenior Contributor
I am a writer, journalist, professor, systems modeler, computational and digital health expert, avocado-eater, and entrepreneur, not always in that order.

With the COVID-19 coronavirus pandemic, ventilators, like this one seen next to an intensive care ... [+] DPA/PICTURE ALLIANCE VIA GETTY IMAGES
Suffice it to say that the COVID-19 coronavirus is not a very good guest.
It has been the uninvited guest in over 287,239 humans to date based on reported cases. But the actual number is probably many more than that. It has resulted in a pandemic, which is a bad thing for a guest to do. And the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) has proven that it can kill, having claimed at least 11,921 lives as of today, according to a Johns Hopkins University website. But obviously the virus doesn’t have little teeth or carry teeny-weeny sticks of dynamite. So, what exactly does the virus do once it is in your body and how can it kill?
The SARS-CoV2 is a respiratory virus, meaning that it can enter and invade your respiratory system, the system from your nose to your lungs that allows you to breathe in oxygen and breath out carbon dioxide. There are many other kinds of respiratory viruses such adenoviruses, rhinoviruses, respiratory syncytial viruses (RSV), influenza, and other coronaviruses because your respiratory tract can seem like a wet, warm Walmart for these viruses. Some of these viruses tend to stay in your upper respiratory tract while others may make it down to your lower respiratory tract. Spoiler alert: SARS-CoV2 can do both.
Of note, just because two different types of viruses are both considered respiratory viruses, doesn’t mean that they are the same in other ways. The many viruses that cause the common cold including four other types of coronaviruses (OC43, HKU1, NL63, and 229E) behave very differently from the SARS-CoV2. Similarly, the SARS-CoV2 is not the same as the flu virus. Repeat, they are not the same. If you were to ask whether the flu and COVID-19 were equivalent, the answer would be no times no. As Yoda would say, the same they are not SARS-CoV2 and the influenza virus.
SARS-CoV2 gets into your respiratory tract when you breathe in respiratory droplets that have the virus or smear the virus on your face with your grubby fingers or some other contaminated object. The infection tends to begin inside your nose, you know that place in which you may periodically put your finger. The virus looks a little like either a morning star, one of those spiked medieval weapons, or a spiky massage ball. Note that even though the three of these things look similar don’t ever confuse them and use one for the other. The moment someone want to massage you with a weapon or a coronavirus, leave the spa.
Today In: Healthcare
Here is a illustration of the virus that’s causing a pandemic:
This is an illustration of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). (Image: ... [+] GETTY
PROMOTED
And for your reference, here is a spiky massage ball, which is not causing a pandemic:

This is a spiky massage ball. (Photo: Getty) GETTY
The spikes on the surface of the virus consist of protein. Here’s an example of where protein is not good for you. These protein spikes are the key to the viruses’ ability to invade the cells in your respiratory tract. They help the virus find and bind to ACE2, a protein on the surface of your cells that’s the virus’s ace in the hole, so to speak, to get into your cells. This dirt bag virus then tricks your cell into helping it get inside the cell. It uses an enzyme called furin that is present in your cells to break the protein spikes in half, allowing the spikes to then guide the virus into your cells. How’s that for some political backstabbing?
Once inside your cells, the politics don’t end. This jerk virus hijack your cells’ machinery to make more copies of itself. So not only is the virus in your cells’ uninvited, it is doing the nasty there and using your stuff to do so. What a gross creep.
After these pieces-of-bleep viruses make more and more of themselves, they may invade additional cells lining your respiratory tract and begin to cause damage. They may have been able to get into your cells and knock virus boots for a while before your immune system even recognizes that something was amiss. That’s because your immune system probably has never ever seen anything like SARS-CoV2 before and hasn’t yet had the chance to set up specialized sentries and weapons ready to recognize, catch, and eliminate these filthy viruses. When it comes to SARS-CoV2, your immune system is bit like you were probably like in high school, quite naive and easy to fool, no matter how much energy you had and how many weights you lifted.
Thus, your immune system is likely caught with its virtual pants down, something that may also have happened to you in high school. Your immune system then scrambles to deal with the emergency with no real clear plan specific for SARS-CoV2. It quickly assembles and deploys a bunch of general troops to the lining of your respiratory tract, making it into a battleground.
Your startled immune system may be enough to deal with this douchebag virus if everything remains in your upper respiratory tract, that is above your trachea or windpipe. In such cases, your symptoms will likely resemble those of an upper respiratory tract infection. That is, if you even have any symptoms at all. As I wrote previously for Forbes, a study showed that 17.9% of those infected ended up having no symptoms throughout their infections. Upper respiratory symptoms can include a fever, a sore throat, nasal congestion, or a dry cough. As the World Health Organization (WHO) reported, symptoms begin an average of five to six days after the virus initially infected you with a range of one to 14 days.
You may think, OK, so far, SARS-CoV2 doesn’t sound great but it also doesn’t sound terrible. True, for a large percentage of cases, SARS-CoV2 and its damage remains uptown, north of the trachea. But let’s get down with what can go down when the infection proceeds down your respiratory tract into your respiratory tree and lungs.
Shortness of breath, chest pain or tightness, a deeper cough, and other difficulties breathing can be signs that these sons-of-viruses have made it to your lower respiratory tract. These symptoms can come from inflammation of your respiratory tree, otherwise known as your bronchial tree, the set of pipes that carry the air that you breath in and out of your lungs and allow you to sing Rolling in the Deep.
These sleazeball viruses may not stop at your bronchial tree. At the end of your respiratory tract are a bunch of balloon-like structures. No, not a collection of celebratory balloons to congratulate oxygen for reaching all the way down there. Rather, these are alveoli, which may sound like a pasta dish but instead are membranous structures that fill with the air that you inhale. Here is an illustration of some alveoli:
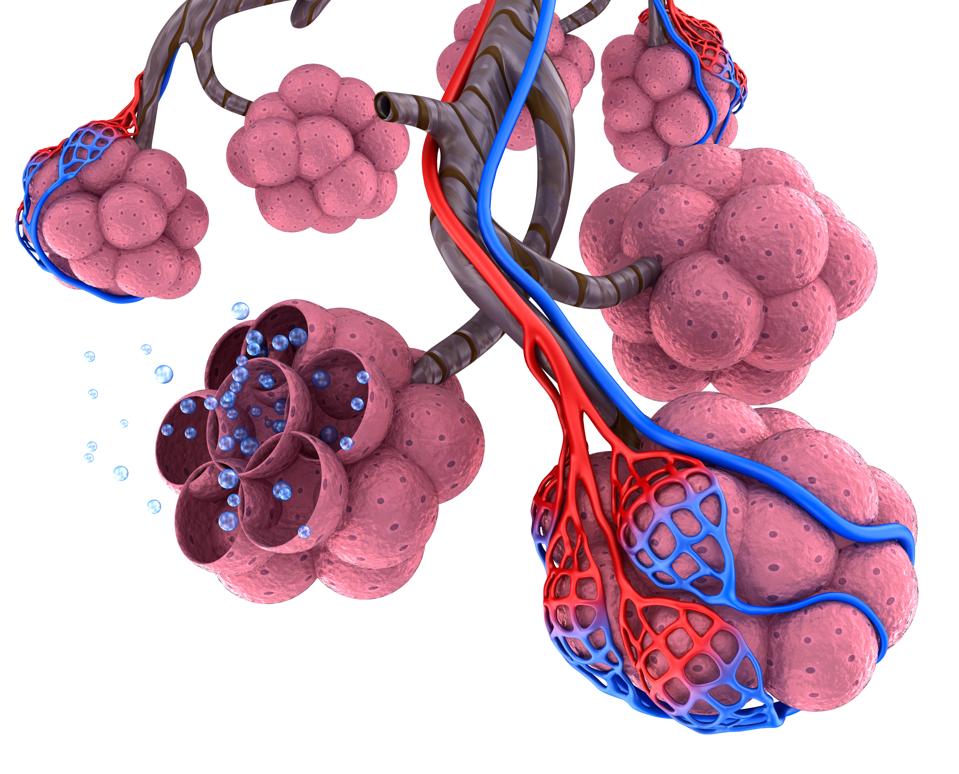
(Image: Getty) GETTY
As you can see in the picture, alveoli are also intertwined with a network of blood vessels, represented in red and blue. These blood vessels bring blood from the rest of your body that is low in oxygen and high in carbon dioxide, a waste product of metabolism. The alveoli serve as swap markets or little eBays where oxygen from the air that you breathed in is exchanged with the carbon dioxide in your blood. The carbon dioxide goes into the alveoli, where it may be exhaled up through your respiratory tract and out through your nose and mouth. The blood that is newly infused with more oxygen subsequently travels to the rest of your body to provide all of your cells with the oxygen that they need to do stuff like live and help you take selfies of yourself.
You can see how your lungs are so important and should be among your top five favorite organs. When your alveoli don’t work properly, your body can become starved of oxygen and unable to get rid of carbon dioxide. Things can quickly go downhill after that happens.
If the viruses and the resulting battle make it down to your lungs and alveoli, it can become a pneumonia. Pneumonia is when your alveoli become inflamed and get filled up with fluid, pus, and other types of gunk. Gunk is a technical term for cells and other stuff. This can happen in one or both of your lungs, assuming that you have no more than two. Developing a pneumonia is when the infection gets really serious. The word pneumonia should never be followed by no more than “I will just walk it off” or “rude, well that’s annoying.” If you suspect that you have a pneumonia, any kind of pneumonia, contact your doctor immediately.
Of course, unless you have an X-ray machine in your home, you can’t tell for sure if you have a pneumonia. Therefore, be aware of possible symptoms such as a high fever, chills that may be accompanied by shaking, coughing up mucus that’s greenish, yellow, or bloody, chest pain, shortness of breath, and other breathing difficulties. You may also feel tired, have a loss of appetite, and suffer sweating episodes. If you start turning blue or becoming confused, those are signs that you may not be getting enough oxygen through your lungs. Turning blue is never a good sign unless you are a member of Blue Man Group. If you do turn blue, go to the emergency room immediately as opposed to go to the emergency room casually. If you are a member of Blue Man Group, please say something.
When the infection has reached your lungs, your panicked immune system can behave like an adolescent. Sure, your immune system can continue to battle the virus, but it can also be too excitable and thus end up of making matters worse. There can be a lot of, shall we say, premature activation. Your immune system can end up quickly sending more and more troops to the area, cascades of different cells and chemicals, that end up firing all over the place in random directions. This may not even root out the invader and at the same time cause additional damage to the cells in your respiratory tract. As you probably learned in high school, telling someone this frenzied to calm down probably won’t work.
The other problem is that while your immune system is battling this scoundrel virus, other nasty microbes such as bacteria can sneak into your lungs and cause havoc as well. This is analogous to when a bouncer is occupied by an unruly guest and other people are able to sneak into the nightclub. These new invaders then can cause secondary infections that subsequently flourish quickly because your defenses are currently occupied. Such infections can end up being life threatening as well.
As the damage to your lungs continues, you may develop acute respiratory distress syndrome (ARDS), which is when your lungs have suffered so much widespread injury that you start running out of functioning alveoli to do the gas exchange work. The acronym ARDS is easy to remember because it sounds a bit like “argh.” If the damage gets to the point that your lungs can no longer effectively exchange enough oxygen and carbon dioxide, you go into respiratory failure and need a ventilator to help you breathe. In such cases, a ventilator is not an optional thing like dressing on a salad. It is an emergency measure to keep you alive. That’s why doctors are so worried about ventilator shortages right now. When you are in respiratory failure, it’s not as if you can take a number and wait for a ventilator to become available. Being out of ventilators is not the same as being out of stock of Fifty Shades of Grey books or hoodies. People will die without enough ventilators.
Being on a ventilator is still not the worst that can happen. Your immune system, you know that naive adolescent that’s been prematurely randomly firing, can go even more haywire. Real trouble occurs when your immune system begins to send chemicals and cells to not only your lungs but all over your body. The destruction then extends beyond your respiratory tract. The Centers for Disease Control (CDC) describes sepsis as “the body’s extreme response to an infection. It is a life-threatening medical emergency.” Your blood pressure starts to drop, your organs starts to fail. This is DEFCON 1 for your body and possibly a point of no return.
Most people with COVID-19 don’t go down this path. According to the Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19), approximately 80% of those with laboratory confirmed COVID-19 end up having mild-to-moderate disease. Mild disease tend to last about two weeks.

An emergency room doctor in his 40's who worked at EvergreenHealth in Kirkland, Washington, is in ... [+] GETTY IMAGES
However, based on this report, a not insignificant 13.8% of those with laboratory confirmed COVID-19 have severe disease. It can take three to six weeks to recover from severe disease, if you even do recover. Deaths, unfortunately, continue to occur.
So what are the chances of death if you have COVID-19? A CDC Morbidity and Mortality Weekly Report (MMWR) published on March 18 presented data on the 4,226 COVID-19 cases in the U.S. that had been reported to CDC as of March 16. Of these cases, 2,449 of these patients had a known age: 6% were 85 years or older, 25% were between 65 and 84 years old, 18% between 55 and 64, 18% between 45 and 54, 29% between 20 and 44, and 5% between 0 and 19.
As you can see, the cases have spanned the age groups of the adult population. However, the case fatality rate, which is the percentage of cases who ended up dying, was substantially higher for those 85 years and older with 10% to 27% of them not surviving. This obviously sounds very high, but keep in mind that these were cases that were diagnosed and reported to the CDC. Without more widespread testing, it is still unclear how many cases of COVID-19 had already occurred in the U.S. as of March 16. The case fatality rate for those between ages 65 and 84 was 3% to 11%, lower but still quite significant. The case fatality rate dropped to 1% to 3% for those between 55 and 64 years of age and below 1% for those between 20 and 54 years of age. No one 19 years old and below passed away.
So far, case fatality rates have continued to vary somewhat widely. In a press briefing on March 3, WHO Director General Tedros Adhanom Ghebreyesus had said that “Globally, about 3.4% of reported COVID-19 cases have died.” A study that’s currently under review at the journal Nature Research analyzed publicly available data on laboratory-confirmed cases of COVID-19 infections in mainland China and came up with a 1.4% probability of dying from the infection after developing symptoms. Therefore, more data and studies are necessary to resolve these discrepancies in reported case fatality rates.
Regardless, all of the estimates so far remain far above the case fatality rates for seasonal influenza, which tends to be below 0.1%. This new coronavirus may have some similarities to the flu virus in that it is a respiratory virus and can kill you. But it is not the flu. Second verse same as the first, SARS-CoV2 am not the flu. The flu SARS-CoV2 is not. It is indeed something completely new and very different. And that’s the problem.
Follow me on Twitter or LinkedIn. Check out my website.
I am a writer, journalist, professor, systems modeler, computational and digital health expert, avocado-eater, and entrepreneur, not always in that order. Currently, I am a Professor of Health Policy and Management at the City University of New York (CUNY), Executive Director of PHICOR (@PHICORteam), Associate Professor at the Johns Hopkins Carey Business School, and founder and CEO of Symsilico. My previous positions include serving as Executive Director of the Global Obesity Prevention Center (GOPC) at Johns Hopkins University, Associate Professor of International Health at the Johns Hopkins Bloomberg School of Public Health, Associate Professor of Medicine and Biomedical Informatics at the University of Pittsburgh, and Senior Manager at Quintiles Transnational, working in biotechnology equity research at Montgomery Securities, and co-founding a biotechnology/bioinformatics company. My work involves developing computational approaches, models, and tools to help health and healthcare decision makers in all continents (except for Antarctica) and has been supported by a wide variety of sponsors such as the Bill and Melinda Gates Foundation, the NIH, AHRQ, CDC, UNICEF, USAID and the Global Fund. I have authored over 200 scientific publications and three books. Follow me on Twitter (@bruce_y_lee) but don’t ask me if I know martial arts.





Comments